In 1998 there were:
By contrast,
Routine chest x-ray screening often are unable to detect lung cancers until they are of advanced stage.
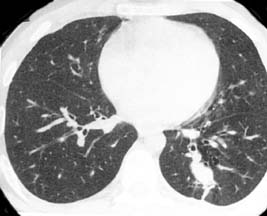
A study by Henschke, et al.found that non-calcified pulmonary nodules were detected in 23% participants by low dose CT at baseline, compared with 7% by chest radiography. Malignant disease was detected in 2-7% by CT and of the 27 CT-detected cancers, 26 were resectable. It was concluded that low-dose CT can greatly improve the likelihood of detection of small (early) lung cancers, and thus potentially more curable stage.
Effective in 2015, Medicare guidelines for low dose CT lung cancer screening are: enrollees must be 55 to 74 years old, have no signs or symptoms of lung disease, and must have smoked at least a pack a day for 30 years or the equivalent — for example, two packs a day for 15 years. They may have quit smoking during the past 15 years, or they may be a current smoker.
Diagnostic Chest CT scans require a prescription by a physician and will only be reimbursed by insurance companies if strict criteria are met. Usually this test is performed if there is an abnormal chest x-ray or history of cancer. Diagnostic CT Scans of the Chest are ordered as a problem solving modality, and usually necessitate intravenous administration of iodinated contrast.
Low-Dose Screening CT is intended to supplement or replace routine CXRs which are performed in patients without symptoms or known disease. Like screening mammography, it is essential to minimize the amount of radiation exposure in asymptomatic patients. The test is specifically designed to rapidly screen the lungs with minimal radiation exposure, to allow detection of pulmonary nodules. No intravenous contrast is used.
Low-Dose Screening CT is specifically designed to screen for pulmonary nodules, and is neither designed nor intended to screen for abnormalities elsewhere in the thorax (ie- heart, aorta, lymph nodes, bones).
You do not need a prescription to obtain this exam. Since this is a screening test, most insurance companies do not reimburse for its cost.
Since it is critical to minimize radiation and to provide complete lung coverage in a breathhold, this test should only be performed on a helical (spiral) CT scanner with current software and hardware upgrades.

First, you complete a brief risk factor questionnaire. Next, you lie down on the imaging table and a CT technologist will ask you to hold your breath while the images are taken. That's it. In twenty seconds, your exam is complete, and you may return to your regular routine. The procedure is pain free, non-invasive, and inexpensive.
Your examination will be overread by two board certified radiologists, and results will be sent to you and your doctor within 48 hours.
If your test was read as negative, then no pulmonary nodules were detected. If you are at high risk for lung cancer, then you should consider repeating the exam yearly.
If the radiologists detected a pulmonary nodule that raises concern, then you will be urged to make an appointment with a lung specialist. You may be asked to return for a diagnostic CT Chest, which is performed with higher spatial resolution and thin cuts through areas of concern, allowing characterization of nodules detected by the screening exam. Frequently, nodules detected on the screening exam are subsequently revealed to be benign granulomas or scars on the diagnostic study. Therefore, an initially positive screening test does not necessarily mean that you have lung cancer.
Call : 561.955.4700
Henschke CI, et al. Early Lung Cancer Action Project: overall design and findings from baseline screening. The Lancet 1999:354:99-105.