
Boca Raton Regional Hospital has on its campus a state-of-the-art whole body PET-CT scanner. This scanner greatly enhances our BRRH oncology program and places us at the cutting edge in the diagnosis and management of cancer patients in South Florida. We are also proud to announce that the Center for Breast Care is one of the few facilities in the country to provide Positron Emission Mammography (PEM), an organ specific high resolution PET scanner which uniquely gives our physicians the capability of functional imaging for breast cancer detection.
PET is a nuclear medicine technique using a camera, which captures powerful images of the human body's function and reveals information of health and disease. Compounds normally existing in the body, like simple sugars, are labeled with radioactive tracers, which emit signals and are injected into the body intravenously. The scanner records the signals that the tracer emits as it journeys through the body and as it collects in targeted organs. A powerful computer reassembles the signals into actual images, which then show biological maps of normal organ function and failure of organ systems in disease.
The reason why PET is so successful is that no other imaging technique shows the internal chemistry of the body so well. Conventional imaging techniques such as X-ray, CAT scans, and Magnetic Imaging Resonance shows anatomy. PET detects chemical and metabolic changes in disease states, such as cancer, before anatomic and structural changes (detected by conventional imaging) have time to develop. Therefore PET can detect diseases when anatomic imaging studies are still normal, and may be informative in differentiating benign from malignant process. PET evaluation of tissue metabolism can indicate the probable presence or absence of malignancy based on differences of biological activity, where as anatomic imaging depends on size and radiographic characteristics of lesions to determine the likelihood of malignancy. In addition, whole body imaging with PET provides a means to examine all the organ systems in the entire body for both primary and metastatic disease in one procedure.
Medicare, as well as many third party payers reimburse for PET because it has been shown that in certain specific disease states PET procedures are cost effective, that is, in certain situations PET is superior to conventional imaging without increasing the cost of the management of these clinical situations. PET has been shown to decrease the cost of diagnostic work-up in the situations listed below by avoiding unnecessary invasive diagnostic and surgical procedures in patients for whom these procedures will have little or no benefit. Given the importance of clinical decisions being made by PET, HCFA recognizes that the quality of image production is a significant concern. Medicare limits coverage of FDG PET to use by high-end full ring dedicated PET scanners such as our PET scanner at Boca Raton Regional Hospital. (Alternative Hybrid PET cameras, such as dual head Gamma Cameras equipped with molecular coincidence detection or Gamma Cameras equipped with 511 KEV collimators have been shown to be vastly inferior in sensitivity and exams performed by these hybrid devices are not approved by Medicare for reimbursement purposes.)
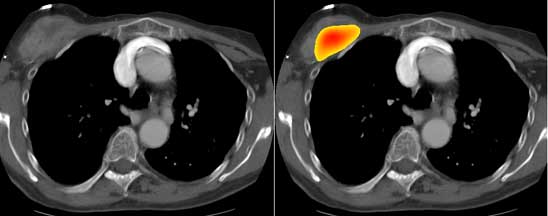
Utilizing a dedicated imaging workstation, we are able to overlay PET data with CT/MRI images, allowing precise localization of tumor.
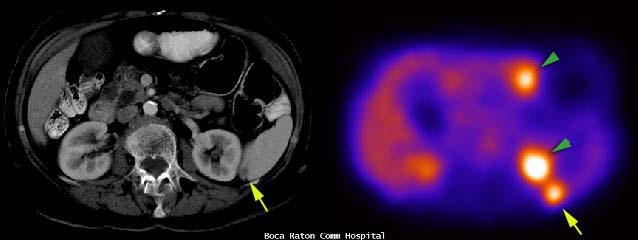
Image fusion readily localized tumor location in the spleen (arrow) in this patient with lymphoma (green arrowheads indicate normal physiologic activity in the bowel and kidney). [CT data above left, PET data above right. Image fusion below.]

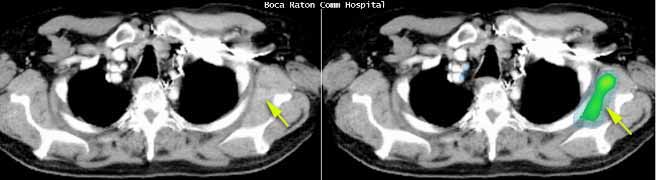
The combined CT & PET data effectively increases specificity and sensitivity of each exam. Lymphoma in the axilla (green on fused CT image of the upper chest on image below) could be easily overlooked when evaluated by CT alone.
A different patient (below) with locoregional recurrence of breast carcinoma along the right anterior chest wall.
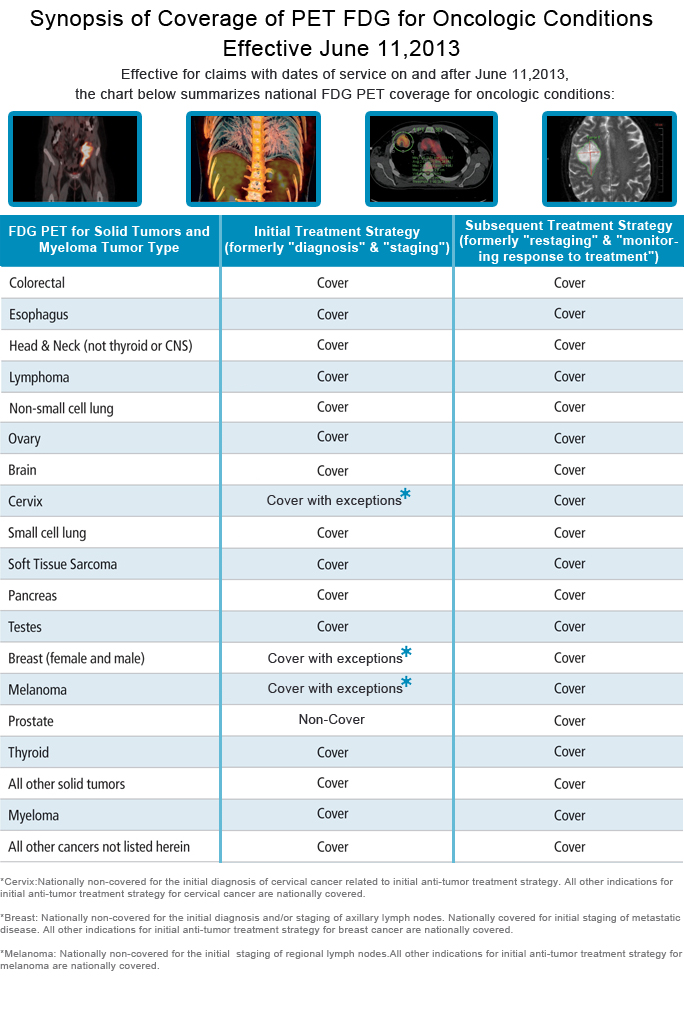
In April 2009, CMS issued a final national coverage determination (NCD) to expand coverage for initial testing with PET for Medicare beneficiaries who are diagnosed with and treated for most solid tumor cancers:
Prior to obtaining an FDG PET study, the physician ordering the procedure is required to document in the patients' chart the specific clinical question that will be answered by the imaging study. The ordering physician will thereby certify the medical necessity of the study according to the conditions described above.
The clinical utility of PET is largely derived from the clinical content in which a physician needs to decide whether to provide or withhold a potentially effective but clearly toxic or risky therapeutic intervention.


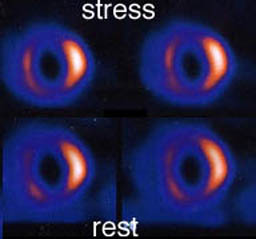
In addition to PET's main role in Oncology it is also used in Cardiology and in Neurology.
In Cardiology, PET has become the 'gold standard' for :
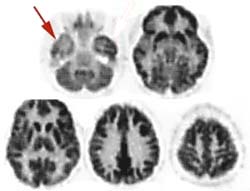
In Neurology, PET plays a vital non-invasive role:
The bottom line is that patients are managed differently when PET is used. Fewer diagnostic and fewer surgical procedures need to be done when PET is used in the diagnostic and surgical work up of patients with primary and recurrent carcinoma. Patients are spared the morbidity and mortality associated with diagnostic and surgical procedures that will have little or no benefit to them, and the insurance companies and the healthcare system are saved the cost of these unnecessary exams.