Cardiac CT & Coronary CTA
Background
The first attempts to image the heart were in the very early days of computed tomography (CT) in the 1970’s. However, due to the rapid motion of the heart and relatively long acquisition times (more than 10 seconds per slice) of early equipment, only large pathological lesions such as tumors along the surface of the heart could be detected. Sub-second slice scanning became possible during the late 1980’s with slip ring (helical) scanners, which utilized a continuously rotating array of detectors and x-ray fan beam around the patient. It became possible to visualize the coronary arteries but not with reliability to diagnose blockages. The first generation slip ring CT scanners used a single row of x-ray detectors but during the 1990’s there were rapid advancements in detector, x-ray tube generators, circuitry, and computers, which allowed the development of multi-row CT scanners. First dual, then four row, then 16 row , then 64 slice CT scanners, and now even faster scanners are available commercially with the speed of image acquisition and volume coverage continuing to increase rapidly with each next generation of CT. The current state of the art CT scanners rotate around the patient between 270 and 500 ms (half of a second). Because the coronary arteries and other cardiac structures move rapidly during the cardiac cycle, data are acquired during cardiac ECG monitoring which allows the computer to then retrospectively reconstruct slices at different small segments of the cardiac cycle and thereby reduce motion artifact in the coronary arteries as well as generate movies of the beating heart thereby assessing valve and wall motion. |
 |
Boca Raton Regional Hospital is proud to have been the first hospital in Palm Beach County to operate a 64 slice CT scanner, and is pleased to be the first in South Florida to operate the Dual Source 128 slice FLASH CT scanner, which is the fastest scanner in the world. We have fellowship trained radiologists with extensive experience and have performed over 5000 cardiac CT scans to date.
Clinical Indications for Cardiac CT
1. Exclusion of coronary artery disease in the low to intermediate risk
patient – It is the best test that is now available with a negative predictive
value approaching 100%. It can visualize early disease before it is detectable
on cardiac catheterization. It may be used to clear patients for surgery
instead of stress testing. Screening is controversial and not supported by
peer reviewed literature.
2. Evaluation for cardiac/pericardial anatomic abnormalities including masses,
thrombus, etc.
3. Triple rule out study for chest pain and can evaluate for other causes
of chest pain including MSK pathology
4. Evaluate status of bypass grafts and stents – are they open? CT may not
be able to fully assess in stent stenosis and grafts with metal clip artifacts.
5. Evaluate wall motion and valve function – this information comes with
extra reconstructions and post processing. Cardiac MRI takes more imaging
time but offers superior capability and without radiation.
6. Detect anomalies including myocardial bridging.
How is the procedure performed?
At the time of scheduling the patient will be asked a series of questions including symptoms, prior history of heart disease and interventions, which will allow us to tailor the examination to answer all of the relevant questions that the referring physician may have. Also, we will need to know if the patient suffers from significant cardiac arrhythmias, which may compromise the quality of the images and diagnostic efficacy.
At the time of the patient’s arrival in our department, the patient will be fully assessed by a cardiac trained nurse (BLS/ACLS certified). The patient’s heart rate, blood pressure, ECG, and history will be reviewed. An intravenous line will be placed into the patient’s arm for fluids and medication. If not contraindicated, we generally administer medications to slow the patient’s heart rate (generally beta-blockers), which improves the image quality and helps ensure a diagnostic study. We will particularly need to know if the patient suffers from asthma or bronchospasm. If beta-blockers cannot be administered, other medications may be used. When the patient’s heart rate is slow and stable, the CT examination is performed which only takes a few minutes including the placement onto the table and the actual image acquisition (done in a breath hold in just seconds). After the examination, the patient is monitored for a short period in our department before discharged.
Applications of Cardiac CT
CT coronary angiography - The most exciting application is the visualization of the coronary arteries which until recently required invasive and dangerous cardiac catheterization. CT should not be directly compared with cardiac catheterization because it offers different and unique information non-invasively. It not only can determine the severity of blockages, but it also directly visualizes the atherosclerotic plaque deposited in the vessel wall. It can identify the early stages of soft (fatty and fibrous) plaque formation even before it can be visualized on x-ray angiography images. It also visualizes calcified plaque, which occurs in more chronic coronary artery disease.
Patients who have already undergone revascularization procedures including stenting and bypass can now be imaged non-invasively.
Due to the rapid improvements in spatial and temporal resolution of the latest generation of CT scanners, there is inadequate scientific review of the state of the art in what is possible in patient diagnosis using this technology. It will undoubtedly change the paradigm of cardiac imaging forever and cardiac catheterization will become a primary therapeutic procedure. With the use of CTA and MRA this has already occurred in other vascular imaging of the body including the carotid arteries, intra-cranial vessels, torso, and extremities.
Current research includes continuing improvements in data acquisition and visualization as well as trying to predict coronary events through the analysis of the type and distribution of the plaque on the CTA examinations.
 |
  |
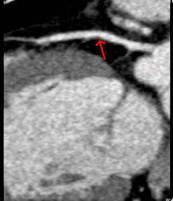
Mild soft plaque of proximal LAD |
Moderate stenosis of LAD and cross
sectional view showing composition of plaque |
 |
 |
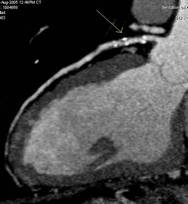
CTA MIP slab proximal right
coronary artery |
Cardiac cath angiogram of same vessel |
| Orange and red arrows show mild
stenoses from soft plaque and yellow arrow reveals proximal moderate
to high grade stenosis secondary to ulcerated lipid plaque, which
was not perceived on selective cardiac catheterization. This
lesion is the most dangerous one and can result in sudden vessel
occlusion and death. |
|
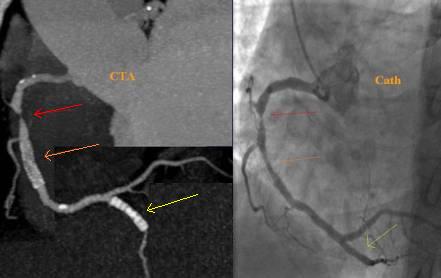 |
Correlation of CTA and cardiac catheterization
using our 64 slice CT. Red arrow points to severe blockage in proximal right coronary artery, orange arrow to proximal stent and yellow arrow to distal (PDA) stent |
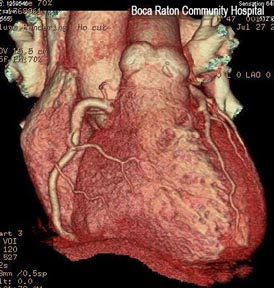
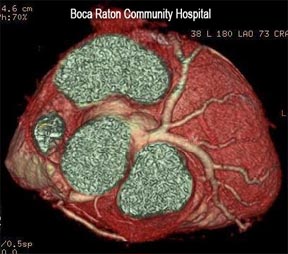
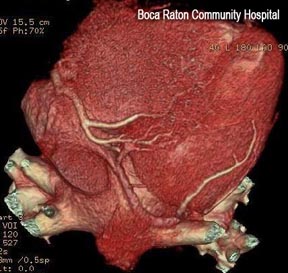
Visualization of cardiac and other structures – because the CT data is volumetric, exquisite structural detail is now possible. Post processing and advanced visualization algorithms allow the extraction of specific structures such as bones, lung tissue, and soft tissue structures, which allows the physician to better understand complex anatomy. This can be invaluable to surgeons in their preoperative planning and very useful in training.
 |
 |
||
 |
 |
||
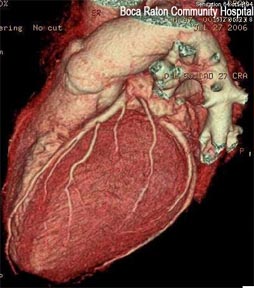
Left lateral, AP, superior and inferior views of heart surface and overlying coronary arteries |
|||
 |
 |
Maximum
intention projection image (MIP) of pulmonary vessels |
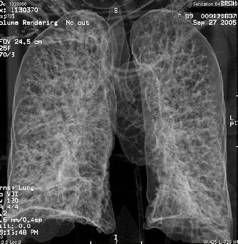
Volume rendered transparency of lungs |
 |
 |
Volume rendering of bony structures of the chest |
Volume rendering of heart the major blood vessels |
Visualization of wall and valve motion – because the CT data is acquired synchronized to the cardiac cycle and the data is volumetric, slices in any arbitrary plane in three-dimensional space can be created during multiple phases of the cardiac cycle. The cardiac function can be assessed non-invasively (like echocardiography and MRI) from the data already acquired for the coronary artery visualization. The only cost is additional computer reconstruction and processing time as well as interpreting physician time. This information otherwise is free. Precise quantitative calculation of ejection fraction can be obtained from these data sets as well as qualitative evaluation of wall motion and valve function. Cross sectional evaluation of valves to measure stenosis is possible.
 |
 |
CTA shows the beating heart. This patient had a previous MI and CABG. Note the normal mitral valve function and the thinned septal wall which shows dyskinesis (motion in wrong direction). |
The beating heart in multiple planes. This case reveals a cardiac tumor within the left ventricle attached to a papillary muscle. (courtesy of the Cleveland Clinic) |
So how does Cardiac CT stack up to existing technology?
Advantages:
1. Quick and non-invasive
2. Three-dimensional modality and is not limited to any particular two-dimensional projections/slice orientation.
3. Can fully assess structures in any plane and offers volumetric information on vessel stenosis and other structures such as cardiac chambers. Can give accurate and unique information of the coronary arteries including narrowing, type and degree of plaque. This may allow more accurate diagnosis and better treatment planning.
4. It is the most sensitive test in detection of coronary artery disease other than intra-vascular ultrasound (IVUS), which requires invasive catheterization of each vessel to its periphery with all of its inherent risks. CTA can non-invasively exclude coronary artery disease.
5. Can also simultaneously visualize the pulmonary and systemic arteries of the chest, thereby excluding other dangerous causes of chest pain including pulmonary embolism and aortic dissection. This is otherwise known as a triple rule out study.
6. Can give accurate information of other structures in the chest, which cannot be otherwise visualized by any other modality such as lung and bony tissue.
7. It is now a 4D modality and can give accurate information of cardiac muscle and valve function and is not limited in visualization or as operator dependent as echocardiography.
Disadvantages:
1. Involves radiation exposure – current generation scanners can now bring the radiation dose to the chest to under 2 mSv which is far less than commonly used in nuclear medicine stress testing.
2.
Has difficulty in patients with fast and particularly irregular heart beats. The images can suffer from registration artifacts and blurring.
3.
Requires iodinated contrast and usually additional medications such as beta-blockers. The risk of these drugs, however, is minimal and we perform this testing in a hospital under close supervision of medical personal.
4.
It can be difficult and occasionally impossible to quantify the degree of luminal narrowing especially in heavily calcified and smaller vessels.
5.
May not be adequate for visualization of plaque and stenotic lesions within certain types of stents and bypass grafts, especially those with heavy metal content and multiple clips.
6.
It may show stenotic lesions as more severe than cardiac catheterization images, which may confuse cardiologists as to the proper course of action. This may actually be secondary to the angiogram under calling the degree of stenosis. (Please see discussion of cardiac catheterization section).
7.
The proper use of this technology is not yet fully understood by cardiologists and there is inadequate scientific literature with outcome analysis as to its true value in diagnostic testing in specific clinical scenarios. Much clinical research is still needed to optimize the diagnostic algorithms in cardiac disease. Also, MRI without requiring ionizing radiation is rapidly evolving and offers similar capabilities in 4D imaging.
 |
 |
Normal aortic valve function (cross sectional). Also note pericardial effusion. |
Normal left ventricular function |
 |
 |
 |
 |
Click on icons to navigate to separate discussion pages including images and movies

