The first attempts to image the heart were in the very early days of computed tomography (CT) in the 1970's. However, due to the rapid motion of the heart and relatively long acquisition times (more than 10 seconds per slice) of early equipment, only large pathological lesions such as tumors along the surface of the heart could be detected. Sub-second slice scanning became possible during the late 1980's with slip ring (helical) scanners, which utilized a continuously rotating array of detectors and x-ray fan beam around the patient. It became possible to visualize the coronary arteries but not with reliability to diagnose blockages. The first generation slip ring CT scanners used a single row of x-ray detectors but during the 1990's there were rapid advancements in detector, x-ray tube generators, circuitry, and computers, which allowed the development of multi-row CT scanners. First dual, then four row, then 16 row , then 64 slice CT scanners, and now even faster scanners are available commercially with the speed of image acquisition and volume coverage continuing to increase rapidly with each next generation of CT. The current state of the art CT scanners rotate around the patient between 270 and 500 ms (half of a second). Because the coronary arteries and other cardiac structures move rapidly during the cardiac cycle, data are acquired during cardiac ECG monitoring which allows the computer to then retrospectively reconstruct slices at different small segments of the cardiac cycle and thereby reduce motion artifact in the coronary arteries as well as generate movies of the beating heart thereby assessing valve and wall motion.
Boca Raton Regional Hospital is proud to have been the first hospital in Palm Beach County to operate a 64 slice CT scanner, and is pleased to be the first in South Florida to operate the Dual Source 128 slice FLASH CT scanner, which is the fastest scanner in the world. We have fellowship trained radiologists with extensive experience and have performed over 5000 cardiac CT scans to date.
At the time of scheduling the patient will be asked a series of questions including symptoms, prior history of heart disease and interventions, which will allow us to tailor the examination to answer all of the relevant questions that the referring physician may have. Also, we will need to know if the patient suffers from significant cardiac arrhythmias, which may compromise the quality of the images and diagnostic efficacy.
At the time of the patient's arrival in our department, the patient will be fully assessed by a cardiac trained nurse (BLS/ACLS certified). The patient's heart rate, blood pressure, ECG, and history will be reviewed. An intravenous line will be placed into the patient's arm for fluids and medication. If not contraindicated, we generally administer medications to slow the patient's heart rate (generally beta-blockers), which improves the image quality and helps ensure a diagnostic study. We will particularly need to know if the patient suffers from asthma or bronchospasm. If beta-blockers cannot be administered, other medications may be used. When the patient's heart rate is slow and stable, the CT examination is performed which only takes a few minutes including the placement onto the table and the actual image acquisition (done in a breath hold in just seconds). After the examination, the patient is monitored for a short period in our department before discharged.
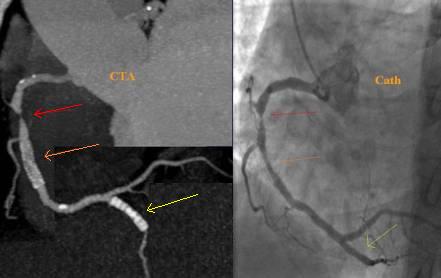
CT coronary angiography - The most exciting application is the visualization of the coronary arteries which until recently required invasive and dangerous cardiac catheterization. CT should not be directly compared with cardiac catheterization because it offers different and unique information non-invasively. It not only can determine the severity of blockages, but it also directly visualizes the atherosclerotic plaque deposited in the vessel wall. It can identify the early stages of soft (fatty and fibrous) plaque formation even before it can be visualized on x-ray angiography images. It also visualizes calcified plaque, which occurs in more chronic coronary artery disease.
Patients who have already undergone revascularization procedures including stenting and bypass can now be imaged non-invasively.
Due to the rapid improvements in spatial and temporal resolution of the latest generation of CT scanners, there is inadequate scientific review of the state of the art in what is possible in patient diagnosis using this technology. It will undoubtedly change the paradigm of cardiac imaging forever and cardiac catheterization will become a primary therapeutic procedure. With the use of CTA and MRA this has already occurred in other vascular imaging of the body including the carotid arteries, intra-cranial vessels, torso, and extremities.
Current research includes continuing improvements in data acquisition and visualization as well as trying to predict coronary events through the analysis of the type and distribution of the plaque on the CTA examinations.


Orange and red arrows show mild stenoses from soft plaque and yellow arrow reveals proximal moderate to high grade stenosis secondary to ulcerated lipid plaque, which was not perceived on selective cardiac catheterization. This lesion is the most dangerous one and can result in sudden vessel occlusion and death.
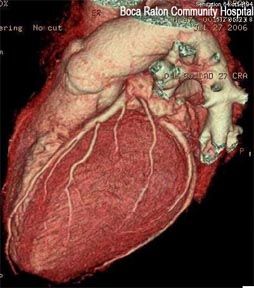
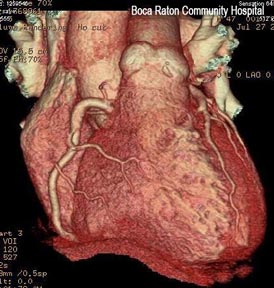
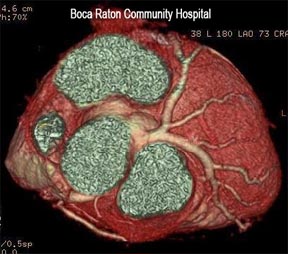
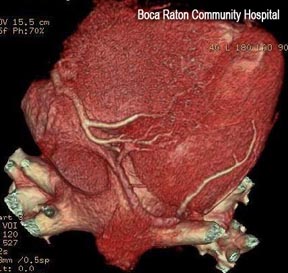
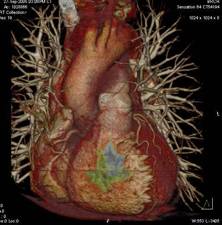
Left lateral, AP, superior and inferior views of heart surface and overlying coronary arteries




Visualization of wall and valve motion – because the CT data is acquired synchronized to the cardiac cycle and the data is volumetric, slices in any arbitrary plane in three-dimensional space can be created during multiple phases of the cardiac cycle. The cardiac function can be assessed non-invasively (like echocardiography and MRI) from the data already acquired for the coronary artery visualization. The only cost is additional computer reconstruction and processing time as well as interpreting physician time. This information otherwise is free. Precise quantitative calculation of ejection fraction can be obtained from these data sets as well as qualitative evaluation of wall motion and valve function. Cross sectional evaluation of valves to measure stenosis is possible.

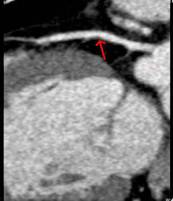
 Normal aortic valve function (cross sectional).Also note pericardial effusion.
Normal aortic valve function (cross sectional).Also note pericardial effusion.
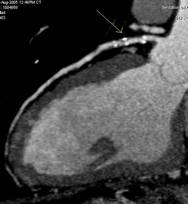
 Normal left ventricular function (short axis view)
Normal left ventricular function (short axis view)