Breast cancer is the most common cancer of American women and the second most common cause of cancer deaths. Extensive breast screening programs are currently effective worldwide. Mammography is the only imaging modality with proven effectiveness in the early detection of clinically occult breast cancer and remains the primary imaging modality for breast cancer screening.
Mammography however suffers with limitations in its ability to detect cancer with a reported sensitivity estimated at 80-85%. This limitation is often due to the obscuration of the tumor by superimposed fibroglandular tissue. Limitations in sensitivity have stimulated the evaluation of adjunctive imaging modalities for breast cancer screening. Breast MRI is one of these imaging tools.
The sensitivity for breast MRI in the detection of invasive breast cancers larger than 3 mm approaches 100%. There is greater variability in the sensitivity in the detection DCIS which ranges from 40-100%.
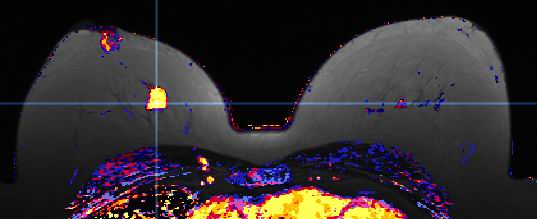
The main strengths of MRI include its exquisite delineation of soft tissue and its ability to image the breast in fine sections dynamically and in multiple planes thereby providing four-dimensional information. The basis of MR enhancement of breast cancer relates to vascularity of lesions and vessel permeability. Invasive breast cancer shows increased vascularity with an increased permeability of this neovascularity leading to an early uptake and early washout phenomenon. Invasive breast cancers tend to have increased vascularity at the periphery leading to a rim-enhancing pattern of lesions. The pattern of enhancement of DCIS can be variable including both ductal and regional enhancement.
Over the last 20 years, advances have been made in the field of breast MRI, however, even today there is no well-defined standard or optimal imaging technique for performing contrast-enhanced breast MRI . Additionally, there are no standardized interpretation criteria and no unified definition of what constitutes clinically important contrast enhancement.
Over the years, there have been 2 major approaches to image interpretation: 1) evaluation of enhancement kinetics or patterns of contrast enhancement 2) evaluation of lesion morphology or appearance. Early researchers from Europe demonstrated that malignant lesions consistently enhance and do so earlier and to a greater degree than benign lesions. Many authors utilized a quantitative approach to kinetic evaluation or enhancement patterns. Others have used a qualitative method for evaluation of the overall shape of the enhancement curve when attempting to distinguish benign from malignant lesions.
Three types of time/enhancement intensity curves have been described. Type I: steady enhancement where a persistent increase in signal intensity is present after 2 minutes . Type II: plateau, where the maximum signal intensity is achieved in 2 minutes and remains constant. Type III: washout, where the maximum achieved signal is demonstrated by 2 minutes and decreases with time. Benign lesions tend to demonstrate Type I curve and malignant lesions Type III.
Lesion morphology or architectural features identified on high spatial resolution images have been used to characterize lesions as to benign or malignant. Features that have been reported as suggestive of malignancy include a mass with irregular or spiculated borders and peripheral or ductal enhancement. Features of benignity include a mass with smooth or lobulated borders, no enhancement, nonenhancing internal septa and patchy parenchymal enhancement. In mammography, lesion margins represent the interface between the lesion and the adjacent parenchyma. The margin interface on MRI represents the interface between the area of vascularity and the surrounding tissue. It cannot be assumed that the mammographic features will necessarily be the same on mammography and MRI.
At the Center for Breast Care we have been performing breast MRI since 2000. We believe an integrated interpretation strategy where enhancement kinetics and morphologic features are used together obtaining superior outcomes compared to the use of either method alone. Despite the fact that there are differing approaches, there is still universal agreement that breast MRI is an extremely sensitive imaging technique for the detection of breast cancer.
Invasive Lobular Cancer : This insidious cancer, difficult to detect by mammography and physical exam is commonly extensive, mutifocal or multicentric and can be bilateral in 10%. Patients with invasive lobular cancer more often have positive margins after lumpectomy. This potentially can be avoided with knowledge gained from preoperative breast MRI.
Breast Cancer Staging : One of the most common indications for breast MRI in our practice is for preoperative staging prior to lumpectomy. The extent of disease and its location is the effected breast and occult disease in the opposite breast will be found. 11% of patients can be expected to have unanticipated cancer in the opposite breast and 18% in the ipsilateral breast. We have found this exam will alter the treatment management in 25% of patients. MRI has a very high negative predictive value meaning that a negative breast MRI significantly improves the confidence that there is no occult invasive cancer in the ipsilateral or contralateral breast.
Occult Breast Cancer : Less than 1% of breast cancers present with malignant axillary nodes but without knowledge of the origin in the breast with normal breast exam and mammography. As the primary tumor is occult, standard treatment has been mastectomy. MRI has successfully located 75% of the primary breast cancers , which can allow treatment with breast conservation surgery.
Positive Surgical Margins : Incomplete resection of tumor results in positive surgical margins in a number of patients post lumpectomy requiring additional resection. MRI can locate residual and or additional tumor for surgical planning.
Neo-Adjuvant Chemotherapy : MRI can document tumor response to chemotherapy both with regards to size and tumor perfusion. Viable tumor however may remain with no abnormal enhancement after chemotherapy.
Post-operative scar vs. tumor recurrence : At 9 months or more after surgery, a mature scar, which may simulate cancer morphologically, does not enhance. Recurrent tumor shows the typical enhancement pattern and will be suspect on MRI.
Implants and known or suspected cancer : The diagnostic capabilities of MRI and ultrasound are not affected by the presence of implants as mammography is known to be. This permits more complete and accurate diagnosis and biopsy planning as needed.
Breast Cancer Screening: Although not currently practiced, several investigational studies are underway evaluating the efficacy of breast MRI in the diagnosis of unsuspected cancer in patients considered at high risk. Patients with a proven predisposition or a strong family history of breast cancer are at increased risk at a much younger age than the general population. Additionally, several pathologies result in increased risk of breast cancer development. These include such diagnosis as atypical ductal hyperplasia, lobular carcinoma insitu, and radial scar. Chest wall mantle radiation to the chest or mediastinum such as performed in patients with lymphoma can increase the risk to develop breast cancer. Certainly, the woman at greatest risk to develop new breast cancer is the patient with a history of breast cancer. In the next year, we would hope to be involved in a clinical investigational study, which would determine the incremental value of breast MRI over clinical exam and mammography in the detection of unsuspected breast cancer in the high-risk woman.
Neo-Adjuvant Chemotherapy : MRI can document tumor response to chemotherapy both with regards to size and tumor perfusion. Viable tumor however may remain with no abnormal enhancement after chemotherapy.
As previously stated, breast MRI has become increasingly important in the detection and delineation of breast cancer in our practice. Many studies and our own experience show that MRI can reveal lesions that are both sonographically and mammographically occult. It is clearly the responsibility of the radiologist not only to detect and classify sub clinical lesions but also to ensure their accurate histologic verification. As tissue diagnosis of suspicious lesions is often required, the ability to perform MR guided breast biopsy or localization is an integral component of a dedicated breast MRI imaging program.
Since 2003, the Center for Breast Care has had the ability to perform MRI guided vacuum assisted breast biopsy utilizing a specialized MR compatible system (SUROS/ADEC). We believe we are able to deliver quantitatively and qualitatively satisfactory tissue specimens similar to the results we have achieved over the years with stereotactic and ultrasound guided breast biopsy. With our localization and biopsy equipment we also have the capability to place a tissue marker at the end of the procedure to document the location of the biopsy, being visible on conventional mammography.
We have encountered several technical challenges when performing MRI guided breast biopsy. There may be variation in the appearance of the lesion seen at the time of biopsy and the diagnostic MRI exam. This may be due to variation in positioning, compression of the breast or phase in the menstrual cycle. If the lesion cannot be definitively identified for biopsy, a follow-up exam is recommended.
Posterior and medial lesions have in the past been difficult to approach on MRI guided breast biopsy. However, with the acquisition of new localization technology (MRI Devices) there should be few inaccessible lesions in the future.
IAnother unique problem faced by the physician performing MRI guided breast biopsy is the "vanishing target" or the fading lesion visibility over time after Gadolinium injection. This should not be a problem once the stereotactic coordinates have been determined for the lesion assuming no lesion movement. Confirmation of needle positioning may be difficult particularly with small lesions due to the signal void artifact caused by the large core biopsy system.
As with any other clinically or technically challenging procedure, the patient should seek out that professional team with the most experience and dedication . At the Center for Breast Care we believe MRI is a relatively new imaging technique which allows almost unlimited sensitivity for the diagnosis of invasive breast cancer. However, this tool can best be used to the advantage of the patient if the small equivocal lesions detected become amenable to histologic evaluation. We have worked hard to bring forward an accurate safe and available program for our patients and their physicians.
click here to see our publication in AJR:
"Assessment of Suspected Breast Cancer by MRI: A Prospective Clinical Trial Using a Combined Kinetic and Morphologic Analysis"