Osteoporosis affects more than 30 million Americans. Compression fractures occur in more than 500,000 patients per year in the US, are more frequent than hip fractures, and often result in prolonged disability. Risk factors include advanced age, Caucasian or Asian race, low weight, diseases such as kidney failure, and medication use such as prednisone. Current preventative measures include calcium and vitamin D supplementation, exercise, smoking cessation, and medications such as biphosphonates. Management includes pain control with acetaminophen (Tylenol), non-steroidals (Motrin), narcotics (Percocet), and bracing. Unfortunately, the compression fractures often progress and develop at other levels resulting in loss of height, disability, and secondary complications from immobilization including pneumonia and pulmonary embolism. Percutaneous vertebroplasty has recently been introduced into the US as an effective therapeutic and preventative treatment for the pain and progressive loss of height in compression fractures.
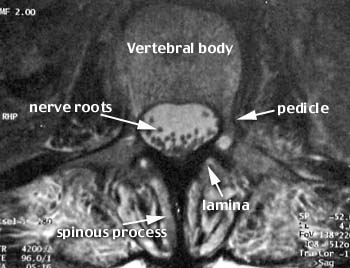
Vertebroplasty literally means fixing the vertebral body. A metal needle is passed into the vertebral body and a cement mixture containing polymethylmethacrylate (PMMA), barium powder, tobramycin, and a solvent are injected under imaging guidance by the physician. The cement hardens rapidly and buttresses the weakened bone. The barium makes the cement visible on x-ray and the tobramycin is an antibiotic. The procedure was originally developed in France in 1984 and has been further refined in the US since 1995.
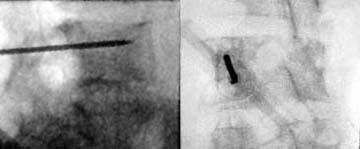
Usually, the procedure is performed in an interventional radiology suite with special x-ray equipment (c-arm fluoroscopy) with nurses and technologists to help sedate the patient and operate the equipment. The patient is placed prone on the x-ray table and made as comfortable as possible. Sedation usually includes a narcotic (fentanyl) and a benzodiazopine (versed), which are short acting and can be reversed if necessary.




.jpg)


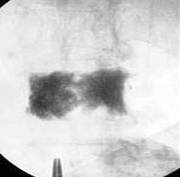
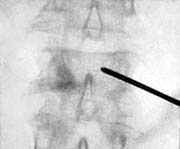
This patient suffered from painful compression fractures. One had already significantly collapsed while the other was just starting to collapse.
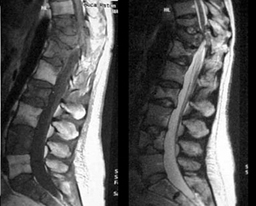
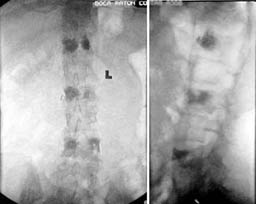
This patient had disseminated metastatic breast cancer to bone and had received both chemotherapy and radiation therapy. She developed paralysis and incapacitating pain. The MRI images show extensive bone tumor with collapse of the T10 and T11 vertebrae resulting in spinal cord compression. There was also extensive tumor in the T12, L2, and L4 vertebrae. Surgery with metal rod stablization was planned but there was fear that further vertebral body collapse would occur. Vertebroplasty was therefore performed at T12, L2, and L4. The patient's paralysis quickly resolved with steroid administration (decreased tumor swelling) and her pain was markedly decreased following the vertebroplasty. She left the hospital without having any surgery.


subspecialty organization committed to excellence in clinical care
research in imaging and therapy of neurological disease